Long term outcomes after autologous bone marrow stem cell treatment in diabetes mellitus: data from unified national electronic health system 2014-2019
Alpamys Issanov1, Arnur Gusmanov1, Yesbolat Sakko1, Dinara Galiyeva1, Raushan Alibekova1, Kainar Kadyrzhanuly1, Kuralay Atageldiyeva1, Askhat Myngbay3, Manarbek Askarov2, Saltanat Tuganbekova2, Byron Crape1, Abay Baigenzhin2, Abduzhappar Gaipov1.
1Department of Medicine, Nazarbayev University School of Medicine, Nur-Sultan, Kazakhstan; 2Department of Medicine, National Scientific Medical Center, Nur-Sultan, Kazakhstan; 3Department of Biology, Nazarbayev University School of Science and Humanities, Nur-Sultan, Kazakhstan
Introduction: Autologous bone marrow stem cell transplantation (ABMT) is one of the promising treatment options in diabetes mellitus (DM). In the 2010s, the Ministry of the Healthcare of the Republic of Kazakhstan (MOH) approved a treatment protocol with ABMT in DM in a single tertiary hospital. However, there is limited data about the long-term all-cause mortality and diabetes-related complications after ABMT compared to conventional treatment (CT). We aimed to study long-term all-cause mortality and diabetes-related complications in DM patients who underwent ABMT versus conventional treatment using large-scale administrative health data from the Unified National Electronic Health System (UNEHS) of MOH.
Methods: The initial cohort of 102,611 patients who were admitted to the hospital with DM were identified using ICD-10 codes through UNEHS between 2014-2019. Out of them, 101 patients who underwent ABMT were defined using ICD-9 procedure codes. Mortality data and patient-related demographics were linked from the National Population Registry. Identified datasets were cross-checked with the whole UNEHS dataset (n=1,565,093 observations) to ascertain the following complications/comorbidities: coronary heart disease (CHD), stroke, retinopathy, nephropathy, neuropathy, diabetic foot, neoplasms. Based on patients’ baseline characteristics (age, sex, duration of DM, residency, ethnicity, number of hospitalizations, and type of diabetes), the cohort of ABMT patients (n=101) matched with a cohort of CT patients (n=102,611) with a 1:5 ratio by propensity score matching (PSM). The final cohort of 601 patients (101 with ABMT vs 500 with CT) was further evaluated.
Results: The baseline characteristics of study cohorts did not differ between ABMT and CT groups after the PSM. The Median (IQR) age of the patients was 27.4 (15.0-43.6) years old, with a median DM duration of 5.8 (4.1-8.9) years. The cohort consisted of 48.8% males, 15.6% rural residents, 79.9% of Kazakh ethnicity, and 57.4% of type 1 DM. The median number of hospital admissions was 3 (2-7) per patient during 2014-2019.
The results of diabetes-related events and all-cause mortality presented in table 1. Patients who underwent ABMT had a 62% lower risk of cardiovascular events compared to CT. All other diabetes-related complications and all-cause mortality except neoplasms were relatively higher in the CT group compared to the ABMT group, however, results were not statistically significant.
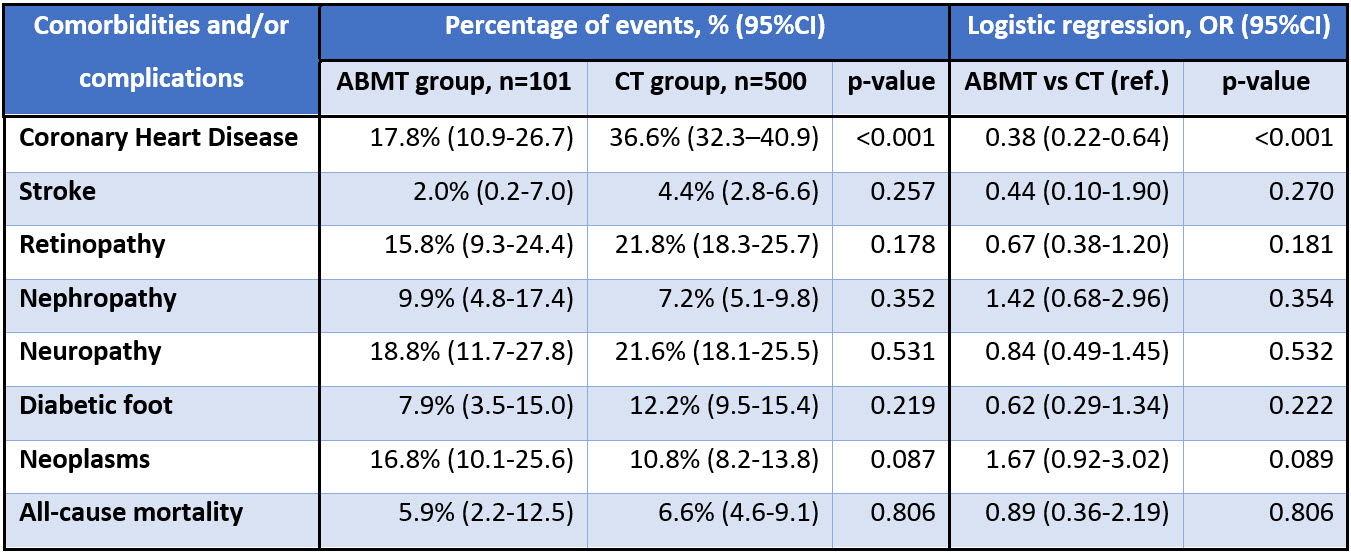
Conclusion: Patients with DM who underwent ABMT had a 62% lower risk of cardiovascular events compared to CT. All-cause mortality and diabetes-related complications except neoplasms demonstrated trends with lower events in ABMT groups, however further investigations needed involving more clinical and laboratory data.
This study was supported by grants from the Nazarbayev University Faculty Development Research Grant Program FDCRGP 2020-2022 (Funder Project Reference: 240919FD3913).