Impact of HLA donor specific antibodies in the era of cell therapy: clinical trajectories in islet allotransplantation illustrate a challenging model
Mehdi Maanaoui1,5, Mikael Chetboun2,5, Isabelle Top3, Julie Kerr-Conte5, Kristell Le Mapihan4,5, Valery Gmyr5, Thomas Hubert5, Myriam Labalette3, Marc Hazzan1, Marie-Christine Vantyghem4,5, François Pattou2,5.
1Department of Nephrology, CHU Lille, Lille, France; 2Department of General and Endocrine Surgery, CHU Lille, Lille, France; 3Department of Immunology, CHU Lille, Lille, France; 4Department of Endocrinology, Diabetology, and Metabolism, CHU Lille, Lille, France; 5U1190 - EGID, Univ. Lille, Inserm, CHU Lille, Institut Pasteur Lille, Lille, France
Introduction: Islet transplantation is a unique paradigm in the case of organ transplantation, since multiple injections and donors are required to achieve complete insulin-independence. Preformed or de novo DSAs may target one or several donor islets, which complexifies the analysis of their impact. Our objective is to discriminate illustrative clinical trajectories which can occur after transplantation.
Methods: Adult type 1 diabetic pancreatic islet recipients transplanted between January 2005 and December 2018, were included in a monocentric observational study. Only patients with available sera tested by Luminex for Class I and II anti-HLA antibodies during their whole follow-up were analyzed.
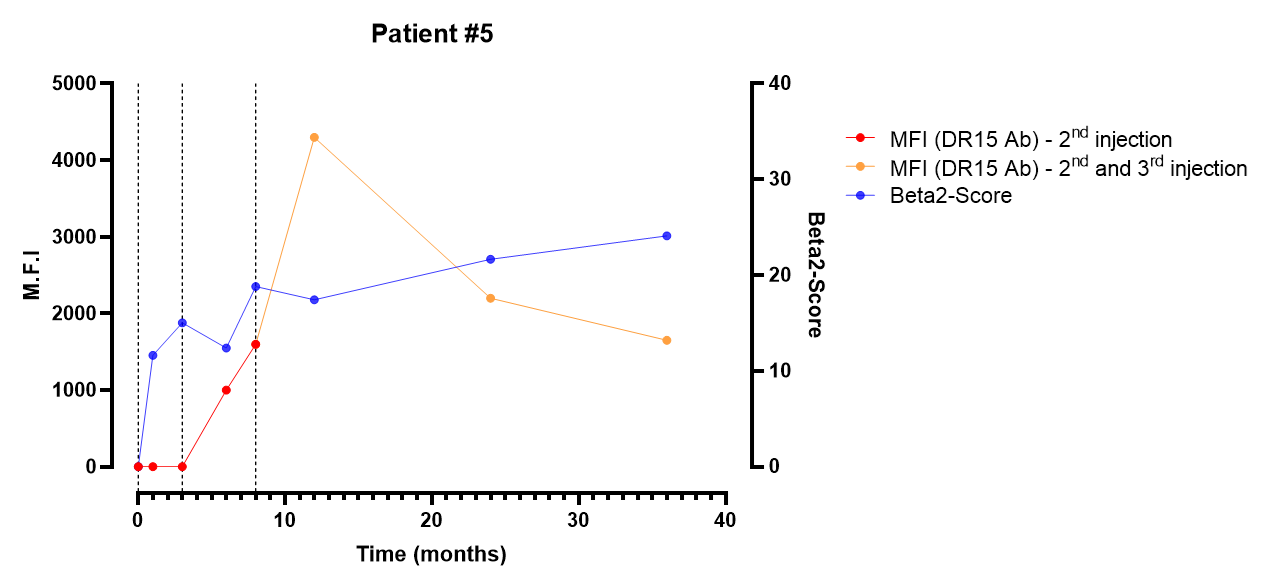
Results: 32 patients had a complete HLA antibodies screening during follow-up. Among them, 7 patients presented with DSA. Five clinical trajectories were identified according to the MFI-value, and the presence of preformed DSA, de novo DSA, or both. To simplify, we provide specific clinical-based trajectories considering an islet transplantation with 1- high MFI preformed DSA, 2- high MFI de novo DSA, 3- low-MFI preformed DSA, 4-low de novo DSA, and 5- a de novo DSA which becomes a preformed DSA because of multiple islet infusions. We analyzed also the specific case of islet-after-kidney transplantation. Recipients transplanted with preformed DSA had all favorable islet transplantation outcomes. The prognosis of de novo DSA was associated with unfavorable outcomes when following markers of unsteady glycemic control.
Conclusion: Clinical-based trajectories and evidence from the literature reveal that islet transplantation with preformed DSA, even with high MFI values, can be associated with favorable outcomes. The fate of recipient presenting with de novo DSA is more questionable as both clinical data and preclinical studies show separate outcomes. Clinical phenotype and unsteady glycemic control before the emergence of DSA may lead the clinician to detect rejection.

I-SITE ULNE.